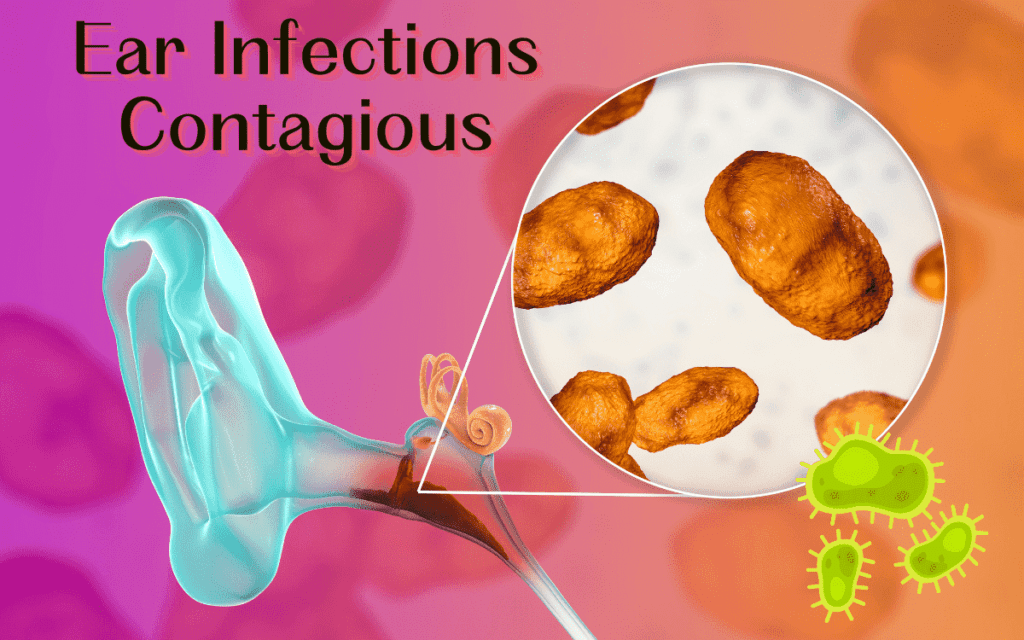
Ear Infections Contagious?
Ear infections themselves are not contagious. However, the underlying causes of ear infections, such as viral or bacterial infections, can be contagious. For example, if someone has a cold or a respiratory infection caused by a virus or bacteria, these pathogens can spread to others and potentially lead to ear infections in susceptible individuals.
Here’s a bit more detail:
Otitis Media: This is a middle ear infection, often resulting from a cold, flu, or respiratory infection that causes fluid to become trapped behind the eardrum.
The bacteria or viruses responsible for these initial infections are contagious, but the ear infection itself is not.
Otitis Externa: Also known as swimmer’s ear, this infection affects the outer ear canal. It’s typically caused by bacteria or fungi and can occur due to moisture remaining in the ear canal after swimming or bathing.
Potential Contagion: If an ear infection progresses to the point of causing a rupture in the eardrum, the discharge (pus or fluid.
The infection itself is not contagious, but the microorganisms causing it can potentially spread in shared water environments.
Understanding Ear Infections
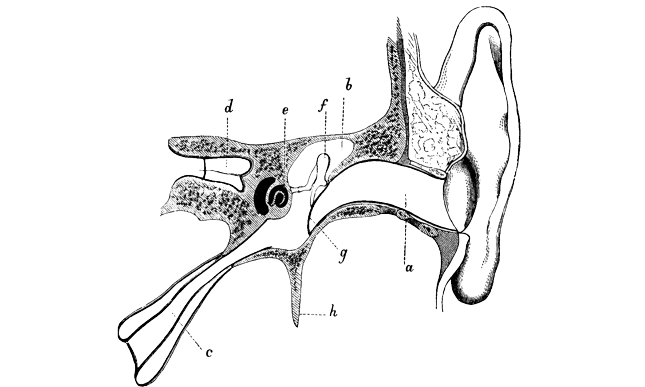
An ear infection, also known as otitis, occurs when a part of the ear becomes inflamed or infected, typically due to bacteria or viruses. It can affect various parts of the ear, including the outer ear, middle ear, and inner ear.
Symptoms may include ear pain, fluid drainage, hearing problems, and sometimes fever.
Different Types of Ear Infections
- Otitis Media (Middle Ear Infection)
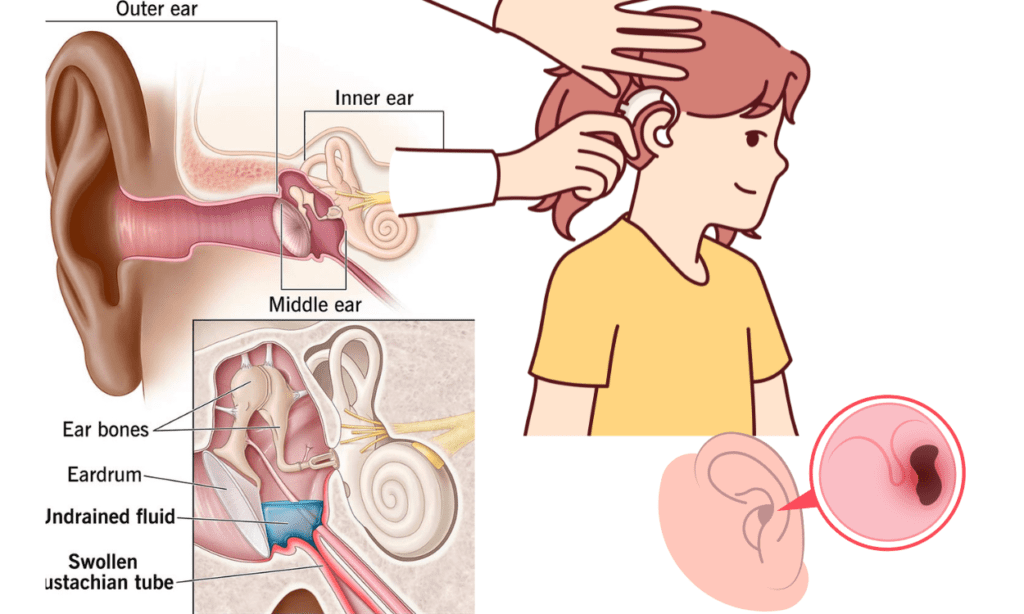
- Description: This type of infection occurs in the middle ear, the area behind the eardrum. It is often associated with colds, respiratory infections, or allergies, which can cause the Eustachian tubes to become swollen and blocked.
- Symptoms: Ear pain, a feeling of fullness in the ear, fluid drainage from the ear, hearing difficulties, irritability in children, and sometimes fever.
- Subtypes:
- Acute Otitis Media (AOM): A sudden infection with symptoms like ear pain and fever.
- Otitis Media with Effusion (OME): Fluid remains trapped in the middle ear after the infection has resolved, leading to a feeling of fullness or hearing loss without acute symptoms.
- Chronic Otitis Media with Effusion (COME): Persistent fluid in the middle ear without infection symptoms, which can impact hearing.
2. Otitis Externa (Outer Ear Infection)
- Description: Also known as swimmer’s ear, this infection affects the outer ear canal, which runs from the eardrum to the outside of the head. It often occurs when water remains in the ear canal, creating a moist environment that promotes bacterial or fungal growth.
- Symptoms: Ear pain, itching in the ear canal, redness, swelling, and sometimes discharge of fluid. Severe cases can lead to significant pain, swelling, and hearing loss.
- Subtypes:
- Acute Otitis Externa: Usually bacterial and occurs suddenly.
- Chronic Otitis Externa: A longer-lasting form that can be due to non-infectious causes like eczema or allergies, or persistent bacterial or fungal infections.
3 Otitis Interna (Inner Ear Infection)
Description: This is less common and involves the inner ear structures, such as the cochlea and vestibular system. It can occur due to viral infections and is often associated with balance and hearing issues.
Symptoms: Dizziness, vertigo, hearing loss, and balance problems.
Causes of Ear Infections
Ear infections often result from a combination of factors that disrupt the normal function of the ear. They can be caused by bacteria, viruses, fungi, or a combination of these pathogens. The development of an ear infection generally follows these steps:
- Initial Infection or Irritation:
- Upper Respiratory Infections: Common colds, flu, or respiratory infections can lead to swelling and congestion in the nasal passages, throat, and Eustachian tubes.
- Allergies: Allergic reactions can cause inflammation and congestion in the nasal passages and Eustachian tubes.
- Blockage of the Eustachian Tubes:
- Swelling and Congestion: Inflammation from infections or allergies can cause the lining of the Eustachian tubes to swell, leading to blockage.
- Structural Issues: In some individuals, particularly children, the Eustachian tubes are more horizontal and narrower, making them more prone to blockage.
- Fluid Buildup:
- Impaired Drainage: When the Eustachian tubes are blocked, they cannot effectively drain fluids that are normally produced in the middle ear. This fluid buildup creates an ideal environment for bacteria or viruses to grow.
- Pressure Changes: Blocked Eustachian tubes can also cause pressure changes in the middle ear, leading to discomfort and pain.
- Infection Development:
- Bacterial or Viral Growth: Fluid trapped in the middle ear can become infected with bacteria or viruses, leading to inflammation and the symptoms of an ear infection.
- Spread from Other Infections: Pathogens from upper respiratory infections can spread to the middle ear, causing otitis media.
The Role of the Eustachian Tubes and Fluid Buildup
The Eustachian tubes play a crucial role in maintaining ear health and function. Here’s a detailed look at their role and the implications of fluid buildup:
- Eustachian Tube Function:
- Ventilation: The Eustachian tubes connect the middle ear to the back of the throat and help equalize air pressure on both sides of the eardrum. This is important for proper hearing and balance.
- Drainage: They also allow normal secretions and any trapped fluids in the middle ear to drain into the throat, preventing fluid buildup.
- Fluid Buildup:
- Blocked Eustachian Tubes: When the Eustachian tubes are blocked due to inflammation, mucus, or structural issues, they can’t perform their drainage and ventilation functions properly.
- Accumulation of Fluids: Fluid that would normally drain out gets trapped in the middle ear. This fluid can become a breeding ground for pathogens, leading to infection.
- Pressure and Pain: The trapped fluid can cause a feeling of fullness, pressure, and pain in the ear. It can also impair hearing by dampening the movement of the eardrum and the ossicles (tiny bones in the middle ear).
Contagiousness of Ear Infections
While the ear infection itself isn’t contagious, the underlying causes and conditions that lead to ear infections can be spread from person to person. Here’s how:
- Viral and Bacterial Infections:
- Upper Respiratory Infections: Viruses or bacteria responsible for colds, flu, sinus infections, or throat infections can spread through airborne droplets (coughing, sneezing) or direct contact (handshakes, sharing utensils). These infections can lead to inflammation in the respiratory tract and Eustachian tubes, which can subsequently cause ear infections (otitis media).
- Allergies:
- Allergic Reactions: Allergens such as pollen, dust mites, mold, or pet dander can trigger allergic reactions in susceptible individuals. Allergies often cause inflammation and congestion in the nasal passages and Eustachian tubes, leading to fluid buildup and increasing the risk of ear infections (otitis media).
- Environmental Factors:
- Smoke and Air Pollution: Exposure to cigarette smoke, air pollutants, or other irritants can irritate the respiratory tract and Eustachian tubes, increasing susceptibility to infections.
- Swimming: Prolonged exposure to water, especially in dirty or contaminated water (like swimming pools), can increase the risk of developing swimmer’s ear (otitis externa), which is caused by bacteria or fungi.
Underlying Contagious Conditions
Respiratory Droplets:
- When an infected person coughs, sneezes, talks, or even breathes, they release respiratory droplets into the air.
- These droplets can contain infectious viruses or bacteria.
- People nearby can inhale these droplets, allowing the pathogens to enter their respiratory tract and potentially cause infection.
Direct Contact:
- Touching surfaces or objects that have been contaminated with respiratory droplets from an infected person can also spread infections.
- If a person touches their mouth, nose, or eyes after touching a contaminated surface, they can introduce the pathogens into their body.
Indirect Contact:
- Some respiratory viruses can survive on surfaces for hours to days.
- People can indirectly pick up these viruses by touching contaminated surfaces (like doorknobs, tables, or shared items) and then touching their face without washing their hands.
Symptoms of Ear Infections
Common Symptoms to Look Out For:
- Ear Pain: This is often the most noticeable symptom, ranging from mild discomfort to severe pain.
- Fluid Drainage from the Ear: In cases where the eardrum has ruptured due to pressure from fluid buildup, pus or clear fluid may drain from the ear.
- Hearing Difficulties: Sounds may be muffled or faint due to fluid accumulation in the middle ear.
- Ear Fullness or Pressure: A sensation of fullness or pressure in the ear can occur.
- Irritability (in children): Infants and young children may show signs of irritability, fussiness, or difficulty sleeping due to ear pain.
- Fever: Sometimes ear infections can cause a low-grade fever, especially in children.
Differences in Symptoms for Children and Adults
Children:
- Tugging or Pulling at Ear: Infants and young children may tug or pull at their ears due to discomfort.
- Difficulty Sleeping: Children may have trouble sleeping, especially lying down, due to ear pain worsening when they are horizontal.
- Fluid Drainage: Children with severe infections may have fluid draining from the ear.
- Irritability: Infants and young children may be irritable or fussier than usual.
Adults:
- Ear Pain: Similar to children, ear pain is a common symptom in adults as well.
- Hearing Issues: Adults may notice a decrease in hearing ability due to the blockage of sound waves caused by fluid in the middle ear.
- Balance Issues: Some adults may experience dizziness or balance problems, especially if the infection affects the inner ear (less common with middle ear infections but can occur).
Prevention Tips
General Hygiene Practices
- Handwashing: Regularly wash hands with soap and water for at least 20 seconds, especially after coughing, sneezing, or touching public surfaces.
- Covering Coughs and Sneezes: Use a tissue or your elbow to cover your mouth and nose when coughing or sneezing to prevent the spread of respiratory droplets.
Preventing Colds and Flu
- Avoid Close Contact: Limit close contact with individuals who are sick to reduce exposure to viruses.
- Stay Home When Sick: If you are sick with a cold or flu, stay home from work or school to prevent spreading the illness to others.
- Boost Immunity: Maintain a healthy lifestyle with regular exercise, adequate sleep, and a balanced diet to support your immune system.
Importance of Vaccinations
- Flu Shot: Getting an annual flu vaccine can reduce your risk of contracting influenza, which can lead to respiratory infections and subsequent ear infections.
Treatment Options
Home Remedies and Over-the-Counter Treatments
- Pain Relief: Over-the-counter pain relievers such as acetaminophen or ibuprofen can help alleviate ear pain and reduce fever.
- Warm Compress: Applying a warm compress to the affected ear can provide relief from discomfort.
When to See a Doctor
- Persistent Symptoms: If symptoms such as ear pain, fever, or hearing difficulties persist or worsen after a few days.
- Fluid Drainage: If there is fluid draining from the ear, indicating a possible ruptured eardrum.
- Severe Symptoms: Severe ear pain, high fever, dizziness, or symptoms that significantly affect daily activities.
Possible Medical Treatments
- Antibiotics: If the ear infection is bacterial, your doctor may prescribe antibiotics to clear the infection.
- Ear Drops: Prescription or over-the-counter ear drops may be recommended to alleviate pain or treat infections (especially otitis externa).
Conclusion
Ear infections, though common, can be managed and prevented with proper hygiene, vaccination, and prompt medical attention when needed. It’s crucial to practice good hygiene to reduce the spread of infections like colds and flu, which can lead to ear infections. Vaccinations, particularly the flu shot, play a vital role in preventing respiratory illnesses that contribute to ear infections.
Early recognition of symptoms and seeking medical advice promptly can lead to effective treatment and reduce the risk of complications. Home remedies and over-the-counter treatments can provide relief from mild symptoms, but persistent or severe symptoms require evaluation by a healthcare professional. Antibiotics and ear drops are common medical treatments for ear infections, depending on the type and severity.