Want to know is asthma an autoimmune disease let’s Explore the facts
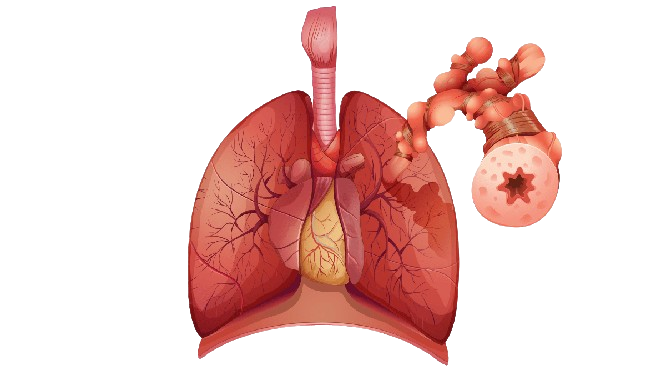
Asthma is a chronic inflammatory condition of the airways in the lungs, characterized by episodes of wheezing, breathlessness, chest tightness, and coughing· It is not an autoimmune disease·
Autoimmune diseases, in contrast, occur when the immune system mistakenly attacks healthy tissues in the body, leading to various conditions such as rheumatoid arthritis, lupus, and multiple sclerosis·
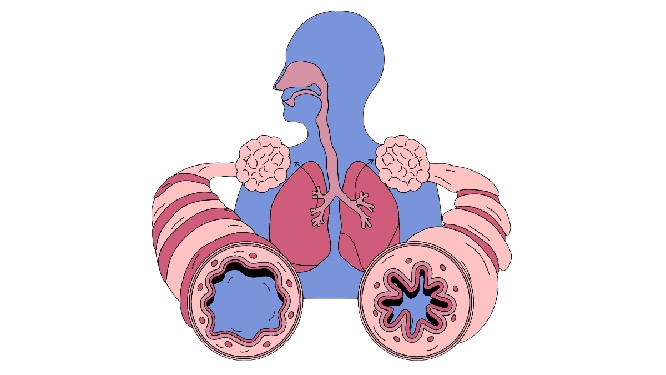
In asthma, the immune system is involved in the inflammation of the airways, but it does not attack the body’s own tissues in the way that occurs in autoimmune diseases·

Is Asthma Considered an Autoimmune Disease
Asthma is characterized as a chronic inflammatory condition of the airways. It leads to symptoms such as wheezing, shortness of breath, chest tightness, and coughing· The inflammation in asthma is triggered by various factors such as allergens or irritants·
Unlike autoimmune diseases where the immune system mistakenly attacks the body’s own tissues, asthma involves an exaggerated immune response to triggers like pollen, dust mites, or pet dander. This immune response causes the airways to become inflamed, narrow, and produce excess mucus, making it difficult to breathe·
Autoimmune diseases, conversely, involve the immune system attacking and damaging healthy tissues. Examples include rheumatoid arthritis, lupus, and multiple sclerosis, where the immune system targets specific self-antigens·
While individuals with asthma may have other health conditions, such as those with autoimmune components, asthma itself is not classified as an autoimmune disease due to its distinct immunological mechanisms and inflammatory pathways.
Potential Links Between Asthma and Autoimmunity
Asthma and autoimmunity share some overlapping aspects, although asthma itself is not categorized as an autoimmune disease:
Asthma is primarily characterized by chronic inflammation of the airways, triggered by various factors such as allergens or irritants· This inflammation leads to symptoms like wheezing and shortness of breath·
Autoimmune diseases involve the immune system mistakenly attacking healthy tissues· Examples include rheumatoid arthritis and lupus, where specific immune responses target self-antigens·
While asthma and autoimmune diseases have distinct immunological mechanisms, some studies suggest potential links. For instance, individuals with asthma may have a higher likelihood of also having autoimmune conditions like rheumatoid arthritis.
Why Asthma is Not Typically Classified as Autoimmune
Asthma is not typically classified as an autoimmune disease due to fundamental differences in how each condition affects the body and the underlying mechanisms involved:
Asthma:
- Inflammatory Condition: Asthma is characterized by chronic inflammation of the airways, triggered by allergens, irritants, or other environmental factors.
- Exaggerated Immune Response: The immune system in asthma responds to these triggers by causing inflammation in the airways, leading to symptoms such as wheezing, coughing, and shortness of breath.
- External Trigger Focus: The immune response in asthma is directed at external stimuli rather than attacking the body’s own tissues.
- Complex Environmental and Genetic Factors: Asthma development is influenced by a combination of genetic predisposition and environmental factors.
Autoimmune Diseases:
- Immune System Misdirection: Autoimmune diseases involve the immune system mistakenly attacking healthy tissues in the body.
- Specific Self-Antigen Targeting: In autoimmune diseases like rheumatoid arthritis or lupus, immune responses are directed against self-antigens, leading to tissue damage and systemic effects.
- Distinct Immunological Pathways: The immunological pathways involved in autoimmune diseases are focused on self-tolerance breakdown and immune dysregulation.
- Clinical and Diagnostic Differences: Medical consensus and diagnostic criteria distinguish asthma as a chronic inflammatory disorder of the airways and autoimmune diseases as conditions involving immune-mediated attacks on self-tissues.
While both asthma and autoimmune diseases involve immune system components, the nature of the immune response and the targets differ significantly between the two conditions. This differentiation is crucial for accurate diagnosis and appropriate treatment strategies tailored to each condition.
Treatment Approaches for Asthma vs. Autoimmune Diseases
Treatment approaches for asthma and autoimmune diseases vary significantly due to their distinct underlying mechanisms and clinical presentations:
Asthma Management Strategies:
Controller Medications: These include inhaled corticosteroids, long-acting beta-agonists, leukotriene modifiers, and mast cell stabilizers. These medications help reduce airway inflammation and prevent asthma symptoms.
Reliever Medications: Short-acting beta-agonists like albuterol are used to quickly relieve acute symptoms such as wheezing and shortness of breath during asthma attacks.
Biologics: These newer treatments target specific immune pathways involved in severe asthma cases. Examples include monoclonal antibodies against IgE (omalizumab), IL-5 (mepolizumab, reslizumab), and IL-4/IL-13 (dupilumab).
Lifestyle Modifications: Avoiding triggers (e.g., allergens, smoke), maintaining a healthy weight, and regular exercise can help manage asthma symptoms.
Autoimmune Disease Treatments:
Immunosuppressants: Drugs like methotrexate, azathioprine, and cyclosporine suppress the immune system to reduce inflammation and prevent immune-mediated damage to tissues.
Biologics: Monoclonal antibodies targeting specific molecules involved in autoimmune responses, such as TNF-alpha inhibitors (e.g., adalimumab), IL-6 inhibitors (e.g., tocilizumab), and B cell inhibitors (e.g., rituximab).
Corticosteroids: These are used to reduce inflammation and manage symptoms during flare-ups in many autoimmune diseases.
Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These drugs aim to slow down the progression of autoimmune diseases by targeting the underlying immune dysfunction.
Pain and Symptom Management: Non-steroidal anti-inflammatory drugs (NSAIDs), analgesics, and physical therapy may be used to manage pain and improve function in certain autoimmune conditions.
FAQ
Is asthma an autoimmune disease?
No, asthma is not an autoimmune disease; it’s a chronic inflammatory condition triggered by environmental factors like allergens.
What causes asthma?
Asthma is primarily caused by environmental triggers such as pollen, dust mites, air pollutants, or respiratory infections.
Are there any similarities between asthma and autoimmune diseases?
Both involve aspects of immune system function, but asthma’s inflammation is triggered externally, while autoimmune diseases involve the immune system attacking the body’s own tissues.
What is asthma?
Asthma is a chronic inflammatory condition of the airways that causes episodes of wheezing, breathlessness, chest tightness, and coughing.
Is asthma caused by the immune system attacking the body?
No, asthma is primarily triggered by environmental factors such as allergens, pollutants, or respiratory infections, not by immune system attacks on the body itself.
Can someone have both asthma and an autoimmune disease?
Yes, it is possible for someone to have both asthma and an autoimmune disease, but they are distinct conditions with different underlying mechanisms.
Conclusion
In conclusion, asthma and autoimmune diseases are distinct in their underlying mechanisms and treatment approaches:
- Asthma is characterized by chronic airway inflammation triggered by environmental factors, managed with medications that reduce inflammation and relieve symptoms during exacerbations.
- Autoimmune diseases involve the immune system mistakenly attacking the body’s own tissues, requiring treatments that suppress immune responses and manage systemic inflammation·
Looking ahead, future research directions include:
Precision Medicine: Advancing personalized treatment strategies tailored to individual genetic and environmental factors influencing asthma and autoimmune diseases·
Biological Therapies: Developing innovative biologics targeting specific immune pathways to enhance efficacy and minimize side effects in both conditions.
Environmental Factors: Investigating the role of environmental exposures, microbiome interactions, and lifestyle modifications in influencing disease onset and progression·
Integrated Care Models: Exploring interdisciplinary approaches that integrate respiratory, immunological, and other healthcare disciplines to optimize patient outcomes and quality of life.