Importance of Addressing Mood Disorders in Childhood
Childhood mood disorders are crucial to address early due to their significant impact on development, early intervention, family dynamics, academic performance, social functioning, physical health, and long-term mental health.
Overview of Mood Disorders in Children
An overview of mood disorders in children includes conditions like depression, anxiety ,Stress, and bipolar disorder, affecting emotional well-being, behavior, and social interactions, often requiring early recognition and intervention for optimal management and long-term outcomes.
Types of Mood Disorders in Children
Childhood mood disorders include conditions, characterized by persistent feelings of sadness, irritability, or extreme highs and lows.
Depression: Feeling sad, irritable, or not interested in things they used to enjoy.
Anxiety: Excessive worrying, fearfulness, or avoiding certain situations.
Bipolar Disorder: Mood swings between extreme highs (lots of energy, feeling very happy) and lows (feeling very sad or hopeless).
Disruptive Mood Dysregulation Disorder (DMDD): Severe temper tantrums and irritability that are more intense than expected for their age.
Adjustment Disorders: Emotional reactions to stressful events like moving or family changes, causing sadness, worry, or trouble concentrating.
Other Specified and Unspecified Mood Disorders: Conditions that don’t fit neatly into the other categories but still affect a child’s mood and behavior.
Common Symptoms and Signs
Common symptoms and signs of mood disorders in children include:
- Emotional Changes:
- Persistent sadness or tearfulness
- Irritability or anger outbursts that are more frequent or intense than expected
- Feelings of hopelessness or worthlessness
- Behavioral Changes:
- Withdrawal from friends, family, or activities they used to enjoy
- Changes in appetite or sleep patterns (eating too much or too little, trouble sleeping or sleeping too much)
- Difficulty concentrating or making decisions
- Physical Symptoms:
- Fatigue or lack of energy
- Complaints of headaches or stomachaches without a clear medical cause
- School and Social Issues:
- Decline in academic performance
- Avoidance of school or social situations
- Increased sensitivity to rejection or criticism
- Risk-taking Behavior:
- Engaging in risky behaviors that are out of character, such as reckless driving or substance use (more common in older children and adolescents)
- Physical Complaints:
- Sometimes children with mood disorders may complain of physical symptoms like headaches or stomachaches, which may not have a clear medical cause.
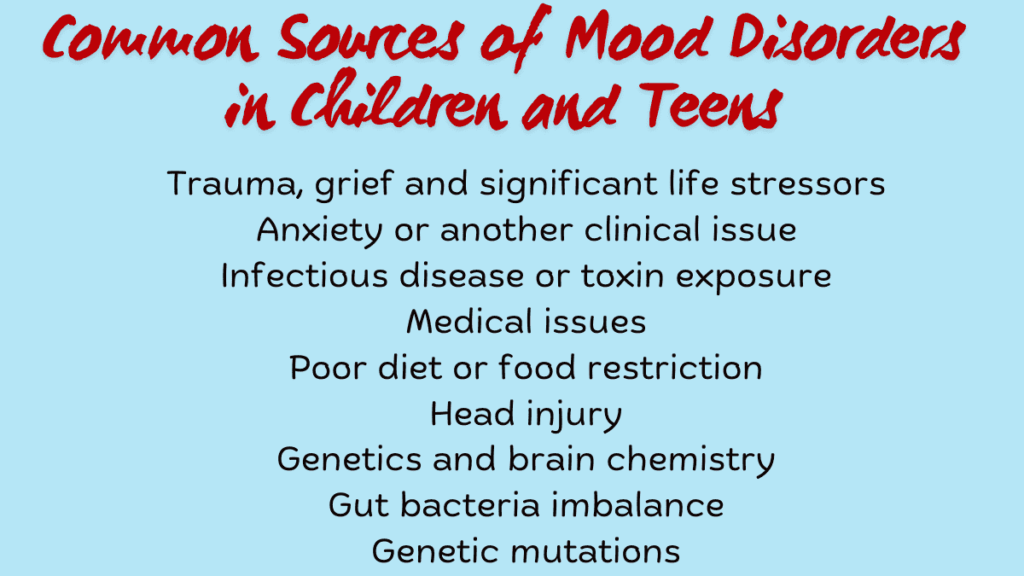
Causes and Risk Factors of Mood Disorders in Childhood
Biological Factors
- Genetics: Children with a family history of mood disorders are at a higher risk. Genetic factors can influence the predisposition to conditions like depression or bipolar disorder.
- Brain Chemistry: Imbalances in neurotransmitters (such as serotonin, dopamine, and norepinephrine) that regulate mood can contribute to the development of mood disorders.
- Hormonal Changes: Changes in hormone levels during puberty or other developmental stages can affect mood regulation and contribute to mood disorders.
- Medical Conditions: Certain medical conditions or illnesses, such as thyroid disorders or neurological conditions, may impact brain function and contribute to mood disturbances.
Environmental Influences
- Stressful Life Events: Traumatic experiences, abuse, neglect, loss of a loved one, or major life changes (such as moving or parental divorce) can trigger or exacerbate mood disorders in children.
- Family Environment: Chaotic or dysfunctional family dynamics, parental conflict, lack of emotional support, or inconsistent caregiving can contribute to emotional instability in children.
- Peer Relationships: Bullying, social rejection, or difficulty forming friendships can impact a child’s emotional well-being and contribute to mood disorders.
- School and Academic Pressure: High academic expectations, performance anxiety, or bullying at school can be stressful factors that contribute to mood disorders in children.
Genetic Predisposition
- Family History: Children with a family history of mood disorders are more likely to develop similar conditions, indicating a genetic predisposition.
- Inherited Traits: Genetic variations and predispositions passed down from parents can influence how a child responds to environmental stressors and their susceptibility to developing mood disorders.
Diagnosis and Assessment Mood Disorders
Challenges in Diagnosing Mood Disorders in Children
- Symptom Variability: Children may express symptoms differently from adults, making it challenging to recognize mood disorders.
- Co-occurring Conditions: Mood disorders often co-occur with other conditions like ADHD or anxiety, complicating diagnosis.
- Developmental Factors: Normal emotional and behavioral changes during development can overlap with symptoms of mood disorders.
- Reliance on Reporting: Children may have difficulty articulating their emotions or may not recognize their symptoms as problematic.
Assessment Tools and Procedures:
- Clinical Interviews: Conducted with the child and family to gather information about symptoms, behaviors, and family history.
- Behavioral Observations: Watching how the child interacts in different settings to assess mood, behavior, and social interactions.
- Questionnaires and Rating Scales: Structured tools completed by parents, teachers, or the child to assess symptoms and functioning.
- Psychological Testing: Cognitive assessments or personality tests may be used to rule out other conditions or assess specific aspects of functioning.
- Collaboration: Multidisciplinary collaboration among healthcare providers, educators, and parents is essential for comprehensive assessment and accurate diagnosis.
Treatment Approaches For Mood Disorders In Childhood
Treatment approaches for mood disorders in children typically involve a combination of therapeutic interventions and, in some cases, medication options.
Therapeutically, Cognitive Behavioral Therapy (CBT) helps children identify and modify negative thought patterns and behaviors contributing to their mood disorders, while play therapy provides a safe space for them to express emotions and learn coping skills through play. Family therapy addresses communication and conflict resolution within the family to support the child’s emotional well-being. Mindfulness-based interventions teach techniques for stress management and emotional regulation.
On the medication front, options include Selective Serotonin Reuptake Inhibitors (SSRIs) for depression and anxiety, mood stabilizers for bipolar disorder, and stimulants for comorbid ADHD and mood disorders, all requiring careful monitoring for effectiveness and side effects.
Individualized treatment plans, regular monitoring, and collaboration among healthcare providers, therapists, educators, and parents are crucial for tailoring interventions to each child’s needs and ensuring comprehensive support.
Support Strategies for Families
Support Strategies for Families:
Supporting families dealing with a child’s mood disorder involves several key strategies:
- Education and Information: Providing families with accurate information about the specific mood disorder their child is experiencing can help them better understand symptoms, treatments, and prognosis.
- Therapeutic Support: Encouraging family members to participate in therapy sessions, such as family therapy, can improve communication, problem-solving, and overall family dynamics.
- Creating a Supportive Environment: Establishing routines and consistent expectations at home can help children with mood disorders feel more secure and supported.
- Encouraging Open Communication: Creating an open and supportive atmosphere where children feel comfortable expressing their feelings and concerns without judgment is essential.
Coping Mechanisms for Parents and Caregivers
- Self-Care: Encouraging parents and caregivers to prioritize their own physical and emotional well-being through activities like exercise, hobbies, and seeking social support.
- Seeking Professional Help: Providing guidance on accessing mental health support for themselves, such as therapy or counseling, to manage stress and emotions related to caregiving.
- Building a Support Network: Connecting with other parents or caregivers facing similar challenges through support groups or online communities can provide validation, advice, and emotional support.
Case Studies and Real-Life Examples
Case studies and personal stories of children with mood disorders offer profound insights into their challenges and the impact of effective treatments.
Take Emma, a 10-year-old girl who struggled with persistent sadness and anxiety, affecting her school performance and social interactions. With support from her family and a therapist, Emma engaged in Cognitive Behavioral Therapy (CBT) and learned mindfulness techniques. Over time, she gained confidence, improved her mood, and developed healthier stress management skills.
Similarly, Jason, a 14-year-old diagnosed with bipolar disorder, experienced extreme mood swings and emotional regulation difficulties. Through a combination of mood-stabilizing medication and family therapy focused on communication and support, Jason’s symptoms became more manageable.
He now participates actively in school activities and has strengthened his family relationships.
In terms of treatment outcomes, Sarah, a 7-year-old diagnosed with major depressive disorder, responded well to SSRIs and play therapy. Her parents observed a reduction in sadness and withdrawal, and Sarah regained interest in activities with friends.
Ethan, aged 12, faced severe anxiety and avoidance behaviors, impacting his daily life. A collaborative approach involving a psychiatrist, psychologist, and school counselor helped Ethan learn anxiety management strategies like gradual exposure and relaxation techniques.
As a result, he became more comfortable in social settings and resumed regular school attendance.
These stories underscore the importance of personalized treatment plans, early intervention, and supportive environments in fostering positive outcomes for children with mood disorders.
They highlight the transformative impact of therapeutic interventions and collaborative care in improving their emotional well-being and overall quality of life.
What are mood disorders in childhood?
Mood disorders in childhood are conditions affecting a child’s mood and behavior, including depression, anxiety, bipolar disorder, and disruptive mood dysregulation disorder (DMDD).
What are the symptoms?
Symptoms include persistent sadness, irritability, loss of interest, changes in sleep or appetite, difficulty concentrating, physical complaints (like headaches), and social withdrawal.
What causes mood disorders in children?
Causes can involve genetics, brain chemistry, and environmental factors such as family dynamics or stressors. These contribute to the development of mood disorders in children.
Conclusion
In conclusion, addressing mood disorders in children is crucial for promoting their well-being and long-term mental health. Throughout this discussion, we have explored various aspects:
Recap of Key Points:
We discussed the importance of early intervention and accurate diagnosis in recognizing and managing mood disorders in children.
Biological factors such as genetics, brain chemistry, and hormonal changes play significant roles, alongside environmental influences like stressors and family dynamics. Effective treatment approaches include therapeutic interventions such as Cognitive Behavioral Therapy (CBT) and medication options like SSRIs and mood stabilizers.
Support strategies for families and caregivers, including education, therapeutic support, and access to resources, are essential for comprehensive care.
Future Outlook and Research Directions:
Looking ahead, future research should focus on enhancing early detection methods, understanding the long-term effects of different treatments, and developing interventions tailored to children’s unique developmental stages.
Collaborative efforts between healthcare providers, educators, and families will be crucial in improving outcomes and supporting children with mood disorders effectively.
In conclusion, by continuing to advance our understanding and treatment approaches, we can better support the mental health needs of children and empower them to lead healthier and more fulfilling lives.
