What is Stage 5 Kidney Failure CKD
Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD) or kidney failure, is the most severe stage of CKD. It is characterized by a significant loss of kidney function, where the kidneys can only filter out a small fraction of waste and excess fluids from the blood.
In Stage 5 CKD
The glomerular filtration rate (GFR), which measures how well the kidneys filter waste from the blood, is less than 15 mL/min/1.73 m². This criterion defines Stage 5 CKD and indicates a critical decline in kidney function (National Kidney Foundation).
Symptoms and complications become severe and typically include fatigue, nausea, swelling (edema), itching, and difficulty concentrating. These arise due to the body’s accumulation of waste products and fluids.
Treatment options include dialysis or kidney transplantation to replace the lost kidney function and maintain the body’s overall health. Dialysis involves filtering waste and excess fluids from the blood artificially, either through hemodialysis or peritoneal dialysis.
Kidney transplantation offers a more permanent solution by replacing the failed kidney with a healthy one from a donor (National Institute of Diabetes and Digestive and Kidney Diseases).
| Stage of CKD | eGFR result | What it means |
| Stage 1 | 90 or higher | Mild kidney damage Kidneys work as well as normal |
| Stage 2 | 60-89 | Mild kidney damage Kidneys still work well |
| Stage 3a | 45-59 | Mild to moderate kidney damage Kidneys don’t work as well as they should |
| Stage 3b | 30-44 | Moderate to severe damage Kidneys don’t work as well as they should |
| Stage 4 | 15-29 | Severe kidney damage Kidneys are close to not working at all |
| Stage 5 | less than 15 | Most severe kidney damage Kidneys are very close to not working or have stopped working (failed) |
Health Risks with Stage 5 CKD
Certainly! Here’s the information about health risks associated with Stage 5 CKD, supported by genuine references:
Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD) or kidney failure, poses significant health risks due to the profound loss of kidney function. Key health risks associated with Stage 5 CKD include:
Cardiovascular Disease Patients with Stage 5 CKD have a markedly increased risk of cardiovascular complications, including heart disease, panic attacks, heart attacks, and strokes.
The kidneys play a crucial role in regulating blood pressure and removing excess fluids, and their dysfunction can lead to hypertension and fluid overload, exacerbating cardiovascular risks (National Kidney Foundation).
Anemia: Decreased kidney function impairs the production of erythropoietin, a hormone essential for red blood cell production. This often leads to anemia, which can cause fatigue, weakness, and other symptoms (National Institute of Diabetes and Digestive and Kidney Diseases).
Bone Disease: Stage 5 CKD can result in mineral and bone disorders due to imbalances in calcium, phosphorus, and vitamin D metabolism. This can lead to bone pain, fractures, and skeletal deformities.
Fluid and Electrolyte Imbalances: The kidneys regulate electrolyte levels (such as sodium, potassium, and calcium) and fluid balance in the body.
In Stage 5 CKD, these functions are impaired, leading to fluid retention, electrolyte imbalances, and potentially life-threatening conditions like hyperkalemia (high potassium levels) or metabolic acidosis
Increased Infection Risk: Impaired immune function and frequent hospitalizations (common in patients undergoing dialysis) increase the susceptibility to infections, including access-site infections in dialysis patients
Mental Health Issues: Chronic illness, frequent medical interventions, and lifestyle changes associated with Stage 5 CKD can lead to depression, anxiety, and decreased quality of life (National Kidney Foundation).
Managing these health risks requires comprehensive care, including close monitoring of kidney function, treatment of complications, lifestyle modifications, and adherence to prescribed therapies such as dialysis or transplantation.
Signs and Symptoms of Stage 5 CKD
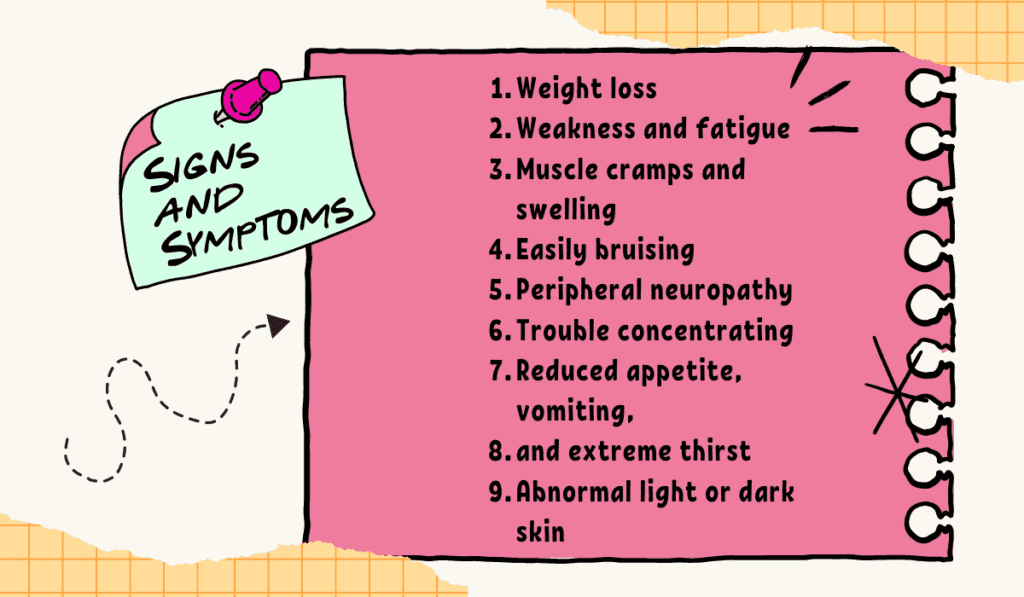
Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD), is the final stage of CKD where the kidneys have lost nearly all their ability to function effectively.
At this stage, dialysis or a kidney transplant is typically required for survival. Here are the signs and symptoms commonly associated with Stage 5 CKD:
- Fatigue and Weakness: Due to the buildup of toxins and waste products in the blood, which the kidneys can no longer effectively filter out.
- Fluid Retention: Swelling (edema) in the legs, ankles, or around the eyes, caused by the kidneys’ inability to regulate fluid balance.
- Decreased Urination: Urination may decrease significantly or stop altogether because the kidneys are no longer able to produce concentrated urine.
- Nausea and Vomiting: The buildup of waste products like urea in the blood (uremia) can cause nausea and vomiting.
- Itching: Accumulation of waste products can cause severe itching, particularly of the skin.
- Loss of Appetite: As a result of nausea, taste changes, and buildup of waste products.
- Metallic Taste in Mouth: Another common symptom of uremia.
- Muscle Cramps and Twitches: Due to electrolyte imbalances, particularly high levels of potassium (hyperkalemia).
- Sleep Problems: Insomnia or restless leg syndrome due to electrolyte imbalances and metabolic disturbances.
- Bone Pain and Fractures: Weakened bones (renal osteodystrophy) due to mineral and hormonal imbalances.
- Easy Bruising and Bleeding: Due to impaired platelet function as a result of uremia.
- High Blood Pressure: Often worsens as kidney function declines.
- Changes in Skin Color: Skin may become darker (hyperpigmentation) or develop a yellowish tint (jaundice) due to the buildup of waste products.
- Difficulty Concentrating and Confusion: Cognitive impairment due to uremic toxins affecting the brain.
- Shortness of Breath: Fluid buildup in the lungs (pulmonary edema) can cause difficulty breathing.
It’s important to note that not all individuals will experience all these symptoms, and some may experience symptoms differently.
Diagnosis of Stage 5 CKD
Diagnosis of Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD), is typically based on several criteria and assessments conducted by healthcare professionals. Here are the key aspects involved in diagnosing Stage 5 CKD:
Glomerular Filtration Rate (GFR): GFR is a measure of how well the kidneys are filtering waste from the blood.
Stage 5 CKD is defined by a GFR less than 15 milliliters per minute per 1.73 square meters of body surface area (ml/min/1.73m²). GFR can be estimated using formulas based on serum creatinine levels, age, sex, and race.
Duration of Kidney Damage: Chronic kidney damage and decreased kidney function should be present for at least three months to qualify as CKD.
Clinical Signs and Symptoms: The presence of symptoms associated with advanced kidney disease, such as fatigue, fluid retention, decreased urine output, nausea, and others mentioned in the previous response.
Imaging Studies: Imaging tests such as ultrasound, CT scan, or MRI may be used to evaluate the structure and size of the kidneys. These can help identify any anatomical abnormalities or signs of kidney damage.
Laboratory Tests: Blood and urine tests are essential to assess kidney function and detect complications associated with CKD. These tests include:
- Serum Creatinine: Used to estimate GFR and assess kidney function.
- Blood Urea Nitrogen (BUN): Measures the amount of nitrogen in the blood that comes from urea, a waste product of protein metabolism.
- Electrolytes (Potassium, Sodium, Calcium): Imbalances in these electrolytes are common in advanced CKD.
- Urine Tests: Analyzing urine for protein (albuminuria), blood (hematuria), and other markers can provide insights into kidney function and damage.
Medical History and Physical Examination: A comprehensive medical history and physical exam help identify risk factors for CKD and assess symptoms and signs of kidney damage.
Underlying Cause Identification: Determining the underlying cause of CKD is crucial as it guides management and treatment decisions. Common causes include diabetes, hypertension, glomerulonephritis, and polycystic kidney disease, among others
Once Stage 5 CKD is diagnosed, further evaluation and management are necessary to determine the appropriate treatment plan. This may include referral to a nephrologist (kidney specialist), initiation of renal replacement therapy (dialysis), evaluation for kidney transplantation, and management of complications associated with advanced kidney disease.
What Causes Stage 5 CKD?
Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD), can result from various underlying conditions and factors that progressively damage the kidneys over time. Here are some common causes and contributing factors:
Diabetes Mellitus: Diabetes is the leading cause of CKD worldwide. High blood sugar levels over time can damage the small blood vessels and nephrons (filtering units) in the kidneys, leading to diabetic nephropathy.
Hypertension (High Blood Pressure): Chronic high blood pressure can damage blood vessels in the kidneys, impairing their ability to filter waste products and maintain fluid and electrolyte balance.
Glomerulonephritis: This refers to inflammation of the glomeruli, which are the tiny structures in the kidneys responsible for filtering blood. Glomerulonephritis can be acute or chronic and is caused by immune system disorders, infections, or other factors.
Polycystic Kidney Disease (PKD): Inherited disorder characterized by the growth of numerous cysts in the kidneys, which can eventually lead to kidney failure.
Autoimmune Diseases: Conditions such as lupus (systemic lupus erythematosus) and other autoimmune diseases can cause inflammation and damage to the kidneys.
Obstructive Nephropathy: Conditions that cause obstruction of the urinary tract, such as kidney stones, enlarged prostate, or tumors, can lead to kidney damage and eventually CKD if not treated promptly.
Recurrent Kidney Infections: Chronic or recurrent infections of the kidneys (pyelonephritis) can cause scarring and damage to kidney tissue over time.
Congenital Abnormalities: Some individuals are born with structural abnormalities in the kidneys that can lead to CKD later in life.
Medications and Toxins: Long-term use of certain medications (e.g., NSAIDs, certain antibiotics) or exposure to toxins and heavy metals can damage kidney tissue.
Vascular Disorders: Conditions affecting blood flow to the kidneys, such as renal artery stenosis or vasculitis, can impair kidney function.
Other Risk Factors: Age, smoking, obesity, and a family history of kidney disease can increase the risk of developing CKD.
It’s important to note that many cases of CKD progress slowly over years or even decades, often without noticeable symptoms until the kidneys are significantly damaged. Early detection through routine screenings and management of underlying conditions are crucial in preventing or slowing the progression of CKD to Stage 5. Once Stage 5 CKD is reached, treatment options such as dialysis or kidney transplantation become necessary to maintain life.
How Can Doctors Determine the Cause of CKD?
Determining the cause of Chronic Kidney Disease (CKD) involves a systematic approach by doctors, often starting with a thorough medical history and physical examination. Here are the steps typically involved:
Medical History: The doctor will ask about your symptoms, medical conditions, family history of kidney disease, medications you are taking, and any other relevant information.
Laboratory Tests:
- Blood Tests: These include serum creatinine, blood urea nitrogen (BUN), and electrolyte levels (such as potassium, calcium, and phosphate). Elevated levels of creatinine and BUN indicate impaired kidney function.
- Urine Tests: Urinalysis and urine protein tests (such as albumin-to-creatinine ratio) help assess kidney damage and detect abnormalities like proteinuria (excess protein in urine).
Imaging Studies:
- Ultrasound: This imaging technique helps visualize the kidneys and urinary tract to identify structural abnormalities like kidney cysts or stones.
- CT Scan or MRI: These may be used for more detailed imaging if ultrasound findings are inconclusive or if a more precise evaluation is needed.
Kidney Biopsy: In some cases, a small sample of kidney tissue may be removed (using a needle inserted through the skin) and examined under a microscope. This is particularly useful when the cause of CKD is unclear from other tests or when the doctor suspects a specific disease affecting the kidneys.
Additional Tests:
- Glomerular Filtration Rate (GFR): This is calculated using serum creatinine levels to estimate how well your kidneys are functioning.
- Genetic Testing: In cases suspected of genetic causes of kidney disease, genetic tests may be conducted.
Identifying Underlying Causes: Based on the results of these tests, doctors can often determine the underlying cause of CKD. Common causes include
- Diabetes mellitus
- Hypertension (high blood pressure)
- Glomerulonephritis (inflammation of the kidney’s filtering units)
- Polycystic kidney disease
- Autoimmune diseases affecting the kidneys
- Congenital abnormalities of the kidneys
- Obstruction of the urinary tract
Treatment and Management: Once the cause of CKD is identified, doctors can recommend specific treatments to slow down progression, manage symptoms, and address underlying conditions contributing to kidney damage.
Determining the cause of CKD is crucial for guiding appropriate management and treatment strategies, aiming to preserve kidney function and improve overall health outcomes.
Treatments for Stage 5 CKD
Stage 5 Chronic Kidney Disease (CKD), also known as end-stage renal disease (ESRD), represents the most severe form of kidney dysfunction where kidneys are functioning at less than 15% of their normal capacity. Treatment options for Stage 5 CKD typically focus on two main approaches:
1. Renal Replacement Therapy (RRT):
Renal replacement therapy becomes necessary when the kidneys can no longer maintain adequate function to sustain life. There are three primary forms of RRT:
- Dialysis: Dialysis is a process that helps to filter waste, excess fluids, and toxins from the blood when the kidneys are no longer able to do so effectively. There are two main types of dialysis:
- Hemodialysis: Blood is filtered through a machine (dialyzer) that performs the functions of the kidneys.
- Peritoneal Dialysis: The lining of the abdomen (peritoneum) acts as a natural filter. Dialysis fluid is introduced into the abdomen through a catheter, and waste products are removed as the fluid is drained.
- Kidney Transplant: A kidney transplant involves surgically replacing the failed kidneys with a healthy kidney from a donor (living or deceased). This offers the best chance for improved quality of life and long-term survival compared to dialysis.
2. Supportive Care and Management:
- Medications: Medications may be prescribed to manage symptoms and complications associated with CKD, such as high blood pressure, anemia, bone disease, and electrolyte imbalances.
- Nutritional Therapy: A dietitian may provide guidance on dietary changes to help manage symptoms and prevent complications. This may involve adjustments in protein intake, sodium, potassium, phosphorus, and fluid intake.
- Management of Complications: Stage 5 CKD increases the risk of various complications including cardiovascular disease, bone disease, anemia, and electrolyte imbalances. Regular monitoring and management of these complications are crucial.
Lifestyle Modifications:
- Exercise: Regular physical activity, tailored to individual capabilities, can help improve overall health and well-being.
- Smoking Cessation: Quitting smoking can help reduce the risk of cardiovascular complications.
- Managing Other Chronic Conditions: Managing conditions like diabetes and hypertension, which often contribute to CKD progression, is essential.
Palliative Care:
For patients who choose not to pursue dialysis or transplant, palliative care focuses on relieving symptoms, improving quality of life, and providing emotional and spiritual support.
Treatment decisions for Stage 5 CKD should be individualized, taking into account factors such as the patient’s overall health, preferences, life expectancy, and potential complications. Nephrologists and multidisciplinary teams play a critical role in guiding patients through these decisions and providing comprehensive care.
Kidney Transplant as a Treatment
Kidney transplantation is a significant medical procedure used to treat end-stage renal disease (ESRD) where the kidneys can no longer function effectively enough to sustain life. Here’s an overview of how kidney transplantation works and its benefits:
Procedure: During a kidney transplant, a healthy kidney from a donor (living or deceased) is surgically implanted into the recipient’s body. The diseased kidneys are usually left in place unless they are causing complications such as infection or hypertension.
Types of Donors:
- Living Donors: Typically family members or close friends who are healthy and willing to donate one of their kidneys.
- Deceased Donors: Kidneys from deceased donors are also used if they are a suitable match for the recipient.
Benefits:
- Improved Quality of Life: A successful kidney transplant can significantly enhance quality of life compared to dialysis.
- Long-term Survival: Generally, kidney transplant recipients have better long-term survival rates compared to those who remain on dialysis.
- No Dialysis: Avoidance of dialysis treatments, which can be time-consuming and have significant lifestyle impacts.
- Improved Health: Kidney function typically improves after successful transplantation, leading to better overall health and reduced complications associated with kidney failure.
Risks and Considerations:
- Immunosuppressive Medications: Recipients need to take lifelong immunosuppressive drugs to prevent rejection of the transplanted kidney, which can have side effects and require careful management.
- Surgical Risks: As with any surgery, there are risks related to the transplantation procedure itself.
- Rejection: There is always a risk that the recipient’s immune system may reject the transplanted kidney, which requires close monitoring and sometimes adjustments in medication.
Post-Transplant Care: After transplantation, regular medical follow-ups are essential to monitor kidney function, manage medications, and watch for any signs of rejection or complications.
Overall, kidney transplantation is considered the best treatment option for many people with end-stage renal disease, offering a chance at a longer, healthier life compared to dialysis. However, it’s important to weigh the benefits against the risks and consider individual factors such as age, overall health, and availability of suitable donors when making decisions about treatment.
Dialysis Options
Dialysis is a treatment option for individuals with kidney failure, also known as end-stage renal disease (ESRD). There are two main types of dialysis:
Hemodialysis (HD):
- Procedure: Hemodialysis involves using a machine (dialyzer) to filter waste products and excess fluids from the blood. Blood is pumped out of the body into the dialyzer, where it is cleaned and then returned to the body.
- Frequency: Typically done three times a week in a dialysis center, each session lasting around 3-4 hours.
- Access: Requires vascular access, usually through an arteriovenous fistula, graft, or central venous catheter.
Peritoneal Dialysis (PD):
- Procedure: Peritoneal dialysis uses the peritoneum (lining of the abdomen) as a natural filter. Dialysis solution (dialysate) is introduced into the abdomen through a catheter, where it absorbs waste products and excess fluids from the blood vessels lining the peritoneum. The solution is then drained out, taking the waste with it.
- Types:
- Continuous Ambulatory Peritoneal Dialysis (CAPD): Manual exchanges done several times a day.
- Automated Peritoneal Dialysis (APD): Uses a machine (cycler) to perform exchanges overnight while the patient sleeps.
- Access: Requires the placement of a peritoneal dialysis catheter in the abdomen.
Comparison and Considerations:
- Flexibility: Peritoneal dialysis offers more flexibility as it can be done at home, whereas hemodialysis is typically performed in a dialysis center.
- Treatment Frequency: Hemodialysis is usually done thrice weekly, whereas peritoneal dialysis can be done daily or nightly.
- Lifestyle: Peritoneal dialysis allows for more independence and fewer restrictions on diet and fluids compared to hemodialysis.
- Complications: Each type of dialysis has its own set of potential complications. For example, hemodialysis can lead to access-related issues or low blood pressure during treatment, while peritoneal dialysis may involve peritonitis (infection of the peritoneum).
Choosing the Right Option:
The choice between hemodialysis and peritoneal dialysis depends on various factors including the patient’s medical condition, lifestyle preferences, vascular access, and support system. Both options aim to manage kidney failure effectively, but the suitability of each method can vary from person to person.
Patients and their healthcare providers typically discuss these factors in detail to determine the most appropriate dialysis modality based on individual needs and circumstances.
Lifestyle Changes and Management Strategies
Managing kidney disease, whether before or after transplantation or while on dialysis, involves several lifestyle changes and strategies to improve overall health and well-being. Here are some key aspects to consider:
Diet and Nutrition:
- Controlled Protein Intake: Adjusting protein intake to manage waste buildup in the blood, which is crucial for both dialysis and pre-transplant care.
- Limiting Sodium: Reducing sodium intake helps manage blood pressure and fluid retention, which is vital for kidney function.
- Phosphorus and Potassium Control: Monitoring and managing phosphorus and potassium levels in the diet to prevent complications such as bone and heart problems.
- Fluid Restriction: Dialysis patients often need to restrict fluid intake to avoid fluid overload and high blood pressure.
- Individualized Plans: Working with a dietitian to create a personalized meal plan tailored to specific kidney needs.
Physical Activity:
- Regular Exercise: Engaging in regular physical activity helps maintain overall health, manage weight, and improve cardiovascular fitness.
- Adapted Activities: Choosing exercises that are safe and suitable for individual fitness levels and medical conditions.
Medication Management:
- Compliance: Ensuring timely and regular intake of prescribed medications, including immunosuppressants post-transplant and medications for blood pressure and other conditions.
- Monitoring Side Effects: Being aware of potential side effects of medications and reporting them to healthcare providers promptly.
Monitoring and Healthcare:
- Regular Check-ups: Attending scheduled medical appointments for monitoring kidney function, managing medications, and addressing any emerging health issues.
- Symptom Awareness: Being vigilant about symptoms such as changes in urine output, swelling, fatigue, and others that may indicate kidney problems or complications.
Emotional and Mental Health:
- Support Network: Building a support network of family, friends, and healthcare professionals to provide emotional support and practical assistance.
- Stress Management: Using techniques like mindfulness, meditation, or therapy to manage stress, which can impact overall health and well-being.
Smoking Cessation and Substance Use:
- Quitting Smoking: Smoking can worsen kidney disease and increase the risk of complications such as cardiovascular disease.
- Avoiding Harmful Substances: Limiting alcohol consumption and avoiding illicit drugs, which can strain kidney function.
Education and Awareness:
- Understanding Kidney Disease: Educating oneself about kidney disease, treatment options, and self-management strategies.
- Advocacy and Support Groups: Participating in support groups or patient advocacy organizations to learn from others’ experiences and access resources.